2,241 Patients Per GP: England's Primary Care Reaches Breaking Point
Record consultations and funding shortfalls leave surgeries unable to hire amid rising risks
A 16% rise in patient loads over a decade, coupled with chronic underfunding, forces GPs to deliver unsafe care. Government pledges mask fiscal offsets that block recruitment, deepening NHS frontline collapse.
Commentary Based On
The Guardian
Dangerous shortage of medics threatens safe patient care in England, top GP says
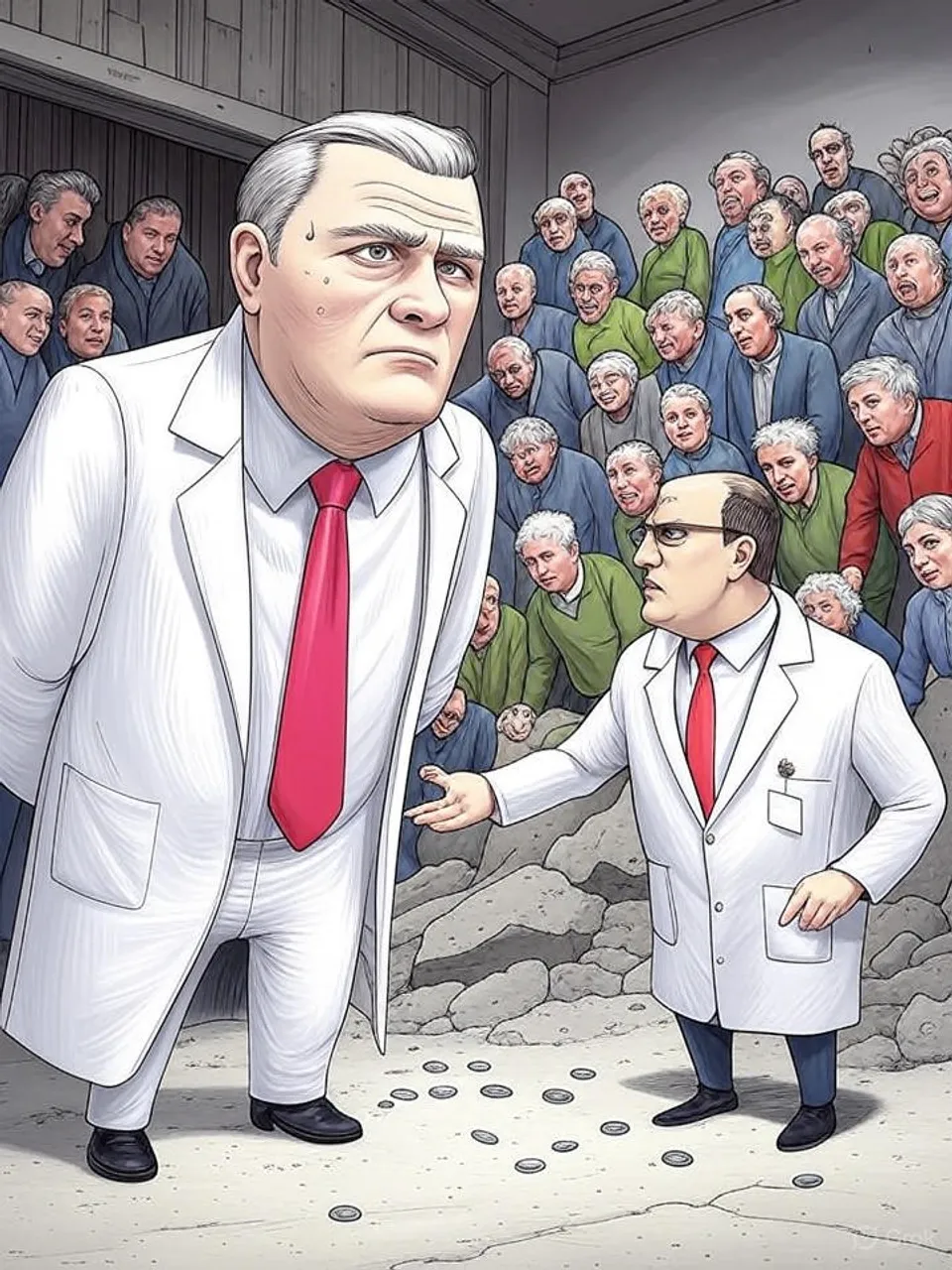
GPs in England now oversee 2,241 patients each, a 16 percent increase over the past decade, as family doctors warn that this caseload directly endangers patient safety. Prof Kamila Hawthorne, chair of the Royal College of GPs, states that surgeries lack the funds to hire additional medics despite desperate need. The gap widens between record consultation volumes and shrinking workforce capacity, turning general practice into a frontline of institutional strain.
Hawthorne’s assessment draws from a survey of GP practice managers. Sixty-one percent of practices require at least one more full-time GP within the next year to manage demand. Yet 92 percent of those managers cite insufficient core funding as the barrier to recruitment.
Consultation numbers underscore the pressure. In the 12 months to September 2025, English GPs delivered 386 million appointments, equivalent to over one million daily and 86 million more than in 2019. This surge coincides with an ageing population presenting more complex conditions, yet patient access remains restricted, with many unable to secure timely slots.
Funding shortfalls trace back decades. Chronic underinvestment has eroded general practice, leaving fewer doctors to handle rising workloads. The result manifests in exhausted staff working unsafe hours, heightening risks of missed diagnoses for serious errors or overlooked deadly conditions.
Government Measures Fall Short
The Department of Health and Social Care points to recent actions: recruitment of 2,500 GPs, elimination of half of administrative targets, and an additional £1.1 billion in funding. These steps aim to alleviate burdens on practices. However, the Royal College disputes their impact, noting that a rise in national insurance contributions offsets the gains.
Eighty-three percent of practice managers in the RCGP survey identify the NIC increase as a key factor blocking new hires. One anonymous manager described the shift: availability of candidates now exists, but financial constraints prevent employment. This dynamic reveals how fiscal policies inadvertently deepen the crisis.
Grassroots discontent escalates. Over 8,000 GPs signed a letter to Health Secretary Wes Streeting, demanding investment in training, recruitment, and retention to restore safety. At a recent conference, GPs voted to resist new online access mandates starting October 1, labeling them unfunded and unsafe amid workforce collapse.
These mandates require surgeries to maintain open online platforms for non-urgent requests throughout working hours. The motion passed by local medical committees condemns the policy as politically motivated, ignoring the reality of stretched resources. Compliance would further overload systems already at breaking point.
Patterns of Persistent Underinvestment
This shortage extends beyond general practice. The NHS relies heavily on foreign staff, yet policies like extended settlement periods for migrants risk driving away 46,000 nurses, as noted in prior analyses. General practice mirrors this dependency, with domestic training pipelines failing to keep pace.
Cross-party governance bears equal responsibility. Successive administrations since the 1990s have promised workforce expansions but delivered incremental gains at best. The current 10-year health plan lacks specific numbers on GP recruitment, rendering it a vague commitment rather than a blueprint.
Accountability gaps compound the issue. Officials announce funding boosts without addressing structural voids, such as procurement inefficiencies or benefit claim surges that divert resources. Practices absorb the fallout, compromising care for millions while ministers tout progress.
The implications ripple outward. Patients face delayed interventions for chronic illnesses, eroding trust in primary care. Economic inactivity tied to health issues already idles nine million working-age adults; untreated conditions in general practice will exacerbate this, straining broader public finances.
Hawthorne calls for a detailed roadmap with concrete figures. Without it, the cycle continues: demand outstrips supply, safety erodes, and staff attrition accelerates. Functional governance would prioritize verifiable workforce targets over rhetorical reforms.
England’s GP crisis exposes the hollow core of NHS sustainability. Decades of underfunding across governments have transformed essential services into rationed necessities, where safe care becomes a luxury. Ordinary citizens pay the price in health risks and inaccessible support, as institutional promises dissolve into repeated failure.
Commentary based on Dangerous shortage of medics threatens safe patient care in England, top GP says by Andrew Gregory on The Guardian.