The Luxury Care Home Where Elderly Residents Sat in Their Own Urine for Hours
When £1,800 a Week Buys You Neglect: Inside Scotland's Most Complained-About Care Home
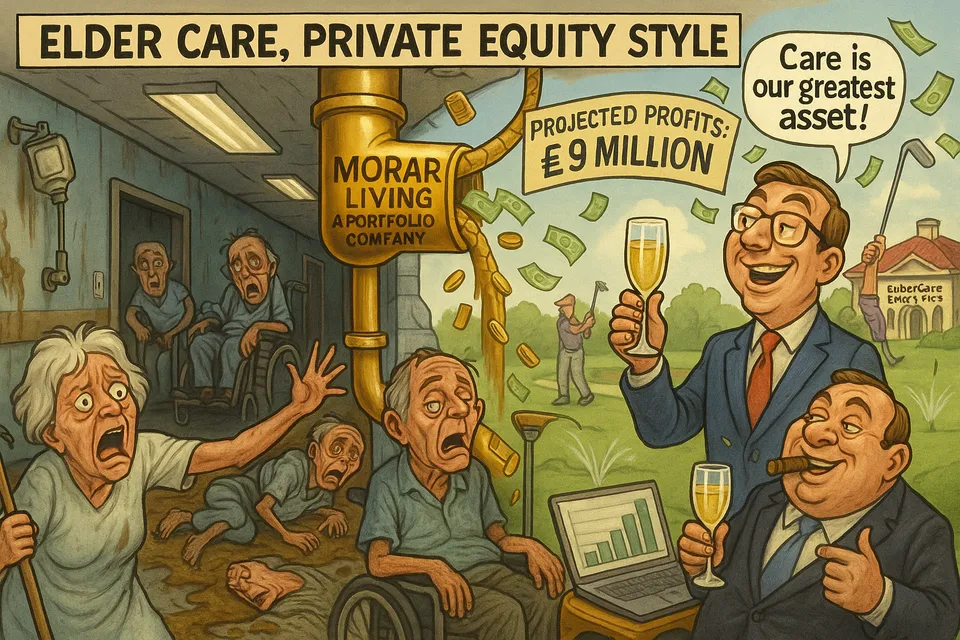
Private equity firm Morar Living expects £90 million in profits over five years while dementia patients scream for help in corridors smeared with excrement. This is the reality of elderly care in modern Britain.
Commentary Based On
BBC News
Families accuse care home of 'neglect' and 'cruelty' after secret filming
While Morar Living projects £90 million in profits over the next five years, its flagship Inverness care home left dementia patients screaming for help in corridors smeared with excrement. This is what happens when venture capital meets vulnerable elderly care in modern Britain.
The Observable Facts
A BBC journalist spent seven weeks undercover at Castlehill Care Home in Inverness this summer, documenting what £1,800 per week actually purchases in British social care. The footage reveals elderly residents left sitting in urine-soaked clothes for hours, women with dementia screaming as male carers performed intimate care against their explicit wishes, and a woman wandering corridors for over an hour with her stoma bag detached, leaving trails of faeces while calling for help.
NHS Highland has transferred almost £10 million in public funds to this facility since 2019. During the BBC investigation period, the home was already under “special measures” following improvement notices from the Care Inspectorate. It continued operating normally.
One resident was secretly filmed being prodded with a walking stick by staff. Another hadn’t been showered for two weeks. Residents sat in chairs for up to eight hours with only a wall-mounted television for stimulation. On one weekend shift, two carers and one nurse were responsible for 23 residents with complex dementia and mobility needs.
The Pattern of Institutional Decay
Castlehill represents something larger than a single failing care home. It demonstrates how British institutions now function: regulatory capture masquerading as oversight, public money flowing to private equity regardless of outcomes, and vulnerable citizens abandoned while bureaucrats issue improvement notices that improve nothing.
The Care Inspectorate knew. They’d rated the home “unsatisfactory” in three key areas in May 2025. They issued improvement notices. They conducted regular checks. They issued more notices with new deadlines. Meanwhile, elderly women continued screaming as male carers violated their documented wishes for female-only intimate care.
This is British regulation in 2025: a performance of oversight that generates paperwork while permitting ongoing harm. The inspectorate “continues to have concerns” and is “monitoring closely.” They’ve been monitoring while a cleaner restrained an elderly man and violently shook his bed frame. They’ve been monitoring while residents developed pressure sores from sitting in wet clothes. They’ve been monitoring while dementia patients tried to escape, sometimes successfully reaching the street.
The Economics of Extraction
Morar Living operates 18 care homes across the UK. Internal documents reveal expectations of £90 million in pre-tax profits over five years and a company valuation exceeding £500 million by 2027. They achieve this by paying carers £13 per hour - the same wage offered by local supermarkets for stacking shelves.
The business model is elegant in its cruelty: extract maximum fees from families desperate to care for vulnerable relatives, minimize costs through skeleton staffing, rely on regulatory inertia to avoid consequences. When caught, promise improvements and hire a “clinical lead” while maintaining the same profit margins.
NHS Highland suspended admissions but continues funding existing residents. The public sector thus remains complicit, transferring taxpayer money to a company that left a woman with dementia screaming in distress for over an hour because reattaching her stoma bag wasn’t profitable enough to warrant adequate staffing.
The Human Cost of Systems Failure
Rachel, a 73-year-old former nurse who spent her life caring for others, explicitly stated she didn’t want male carers performing intimate care. Her family emphasized this to Castlehill management. The home agreed. Then they sent male carers anyway, repeatedly, leaving her screaming in distress behind closed doors.
This wasn’t oversight or miscommunication. It was calculated indifference. With chronic understaffing, the home simply didn’t have enough female carers. Rather than hire more or refuse admissions they couldn’t properly serve, they chose to violate Rachel’s dignity daily while collecting their fees.
Susan Christie found her father sitting in urine when she visited. Her secret camera revealed him left in incontinence pads for over 12 hours, never taken to the toilet, food placed beyond reach. When she complained, staff continued recording in his care notes that he was “sleeping well” and “comfortable” for a full week after she’d removed him from the facility.
The Accountability Void
No one will face meaningful consequences. The cleaner who assaulted a resident with a walking stick was sacked - the minimum possible response to filmed assault. The Care Inspectorate will continue monitoring. NHS Highland will continue funding. Morar Living will achieve its profit targets.
The families who can afford it will move their relatives elsewhere, beginning the cycle again at another home with beautiful pianos in the entrance and cinema rooms that residents never use. Those without resources will endure what the system provides.
Ten upheld complaints made Castlehill Scotland’s most complained-about care home in 2024. This generated no emergency intervention, no criminal investigation, no fundamental restructuring. It generated improvement notices - the regulatory equivalent of strongly-worded letters to organizations extracting millions while elderly people sit in their own waste.
What Competent Governance Would Look Like
A functioning state would have immediately assumed control of any facility where vulnerable citizens were being systematically neglected. Criminal investigations would target not just individual abusers but executives who created conditions enabling abuse through deliberate understaffing. Public funding would be contingent on meeting minimum care standards, verified through unannounced inspections with immediate sanctions for violations.
Instead, Britain operates a Potemkin regulatory system that documents decline without preventing it. The Care Inspectorate observes and reports. NHS Highland expresses concern while continuing payments. Politicians will eventually express shock at conditions everyone knew about, then change nothing substantial.
The Larger Collapse
Castlehill is not an aberration but a manifestation of broader social care collapse. Britain now warehouses its elderly in facilities that generate private profit from public subsidy and private desperation. The generation that rebuilt Britain after World War Two spends its final years sitting in urine while venture capitalists project returns.
This is managed decline made literal: the deliberate, profitable deterioration of citizen welfare while maintaining institutional facades that suggest oversight and standards. Every improvement notice issued without enforcement, every continued payment despite documented abuse, every regulatory observation without intervention represents a choice to permit degradation rather than confront it.
Dr. Jane Douglas, former chief nurse of the Care Inspectorate, acknowledged what everyone knows: “For as long as I’ve worked in the sector, staffing has always been an issue.” This admission of permanent crisis as normal operating procedure captures British institutional culture perfectly. Problems are not to be solved but managed, documented, and monitored while they metastasize.
The Reality Behind the Rhetoric
Political parties compete to promise dignity in old age while presiding over systems that guarantee its opposite. They pledge billions for social care reform that never materializes beyond pilot programs and consultations. Meanwhile, venture capital firms build portfolios from human deterioration, knowing that demographic pressure and regulatory paralysis guarantee profits regardless of performance.
The BBC’s undercover investigation will generate temporary outrage and minor reforms. Castlehill has already appointed a clinical lead and announced £1 million in refurbishments - the standard corporate response to exposed malfeasance. Some families report recent improvements, the predictable temporary uplift that follows public scrutiny before systems revert to profitable dysfunction.
In six months, inspectors will still be monitoring. NHS Highland will still be paying. Elderly residents will still be calling for help that doesn’t come. This is not oversight failure but system design - a conscious choice to prioritize documentation over intervention, process over outcomes, the appearance of standards over their enforcement.
Britain hasn’t failed to create adequate social care. It has succeeded in creating exactly the system its political economy demands: one that extracts maximum value from vulnerability while maintaining sufficient regulatory theater to deflect responsibility. Castlehill is not broken. It’s working precisely as intended.
Commentary based on Families accuse care home of 'neglect' and 'cruelty' after secret filming by Catriona MacPhee on BBC News.