Half a Million Pneumonia Emergencies Overwhelm England's Hospitals Yearly
579,475 cases in one year double the next largest A&E cause, with 97,000 deaths
Pneumonia admissions surged 25% to half a million yearly, exposing decades of neglected respiratory care and deepening NHS overload amid deprivation and absent strategies.
Commentary Based On
the Guardian
Emergency pneumonia cases surge to half a million a year in England
579,475 people required emergency hospitalisation for pneumonia in the year to March 2025. This marks a 25% rise from 461,995 cases two years prior. The figure doubled the next largest cause of A&E admissions.
Pneumonia topped emergency admissions by volume. From April 2022 to March 2025, it killed 97,000 hospital patients. Preventable infections like flu, RSV, and bacterial strains drove most cases.
People with asthma faced three times the pneumonia risk. Those with COPD encountered four times the odds. Existing lung damage eroded natural defences, turning routine infections lethal.
Deprived areas reported 36% higher admission rates. Damp housing, mould, and polluted air weakened residents’ lungs. Basic ventilation gaps amplified viral spread in crowded conditions.
Respiratory care received no dedicated national strategy. Cancer and heart disease claimed priority funding and attention. Primary care sidelined prevention amid daily pressures.
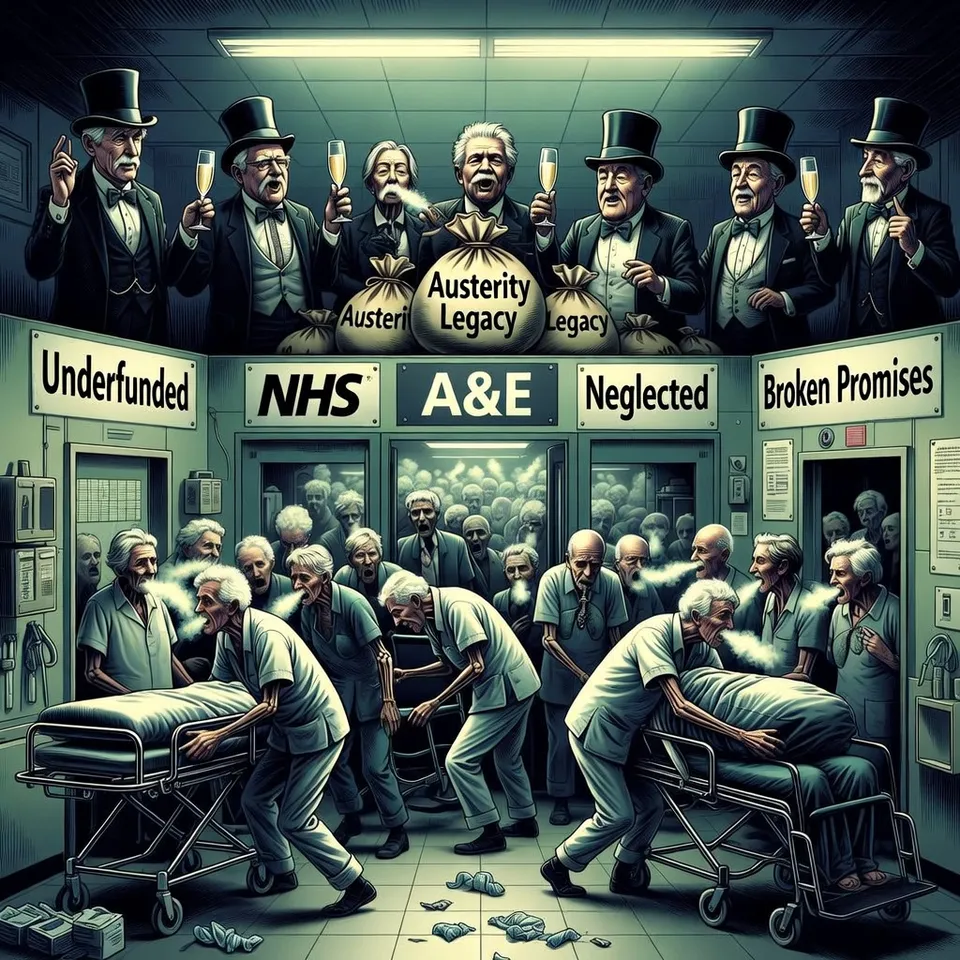
Austerity from the 2010 coalition era elevated pneumonia rates. Numbers dipped only during COVID lockdowns. No government reversed the trend through targeted investment.
Basic care fell short. Just 32% of asthma patients secured full elements like treatment reviews and action plans. COPD patients managed only 8.8%.
Vaccinations lagged. Flu, RSV, and pneumococcal shots prevented escalation, yet uptake suffered. Patients like nurse Sabrina Kaur self-advocated for jabs after near-fatal bouts.
NHS England pledged remote monitoring and community projects. The Department of Health cited a 10-year prevention plan. Delivery remained aspirational as admissions climbed.
Care Gaps Persist Across Governments
Asthma + Lung UK traced neglect to deprioritised respiratory services. Clinicians witnessed avoidable deteriorations. Hospital pressures rose with each untreated case.
Prof Nick Hopkinson noted lung disease’s inequality ties. Global statistics ranked it third in lethality. UK systems ignored the signal.
Historical data showed steady climbs post-2010. Labour’s current term inherited the surge. Structural inertia outlasted party shifts.
Systemic Pressures Mount
Overstretched GPs devalued education and flu shots. Emergency wards absorbed the fallout. Healthcare costs ballooned without upstream fixes.
Deprivation compounded biology. Polluted locales bred susceptible populations. Housing stock decayed without intervention.
Foreign comparisons highlighted underperformance. Functional systems mandated respiratory blueprints. UK’s absence enabled half-million crises.
Patients bore the cost. A 35-year-old nurse coughed blood post-pneumonia. Her conditions worsened despite professional knowledge.
Official responses recycled promises. NHS pilots targeted asthma and COPD. Pneumococcal drives expanded, yet 97,000 deaths accumulated.
Broader Institutional Failure
This surge signalled NHS overload. Pneumonia’s dominance strained beds and staff. Winter peaks loomed without reform.
Public trust eroded as preventable deaths mounted. Voters faced higher taxes for reactive care. Preventive voids drained resources.
Cross-party patterns emerged. Coalitions cut, successors neglected. Incentives favoured crisis management over cures.
Half a million annual pneumonia emergencies reveal respiratory health’s total abandonment. Governments across decades prioritised rhetoric over strategies, leaving lungs to fail and hospitals to fracture. England’s decline embeds in every unvaccinated breath and untreated wheeze.
Commentary based on Emergency pneumonia cases surge to half a million a year in England by Rachel Hall on the Guardian.