NHS Funds Phantom Doctor Shifts for Three Years
£268,000 lost to sick leave scam highlights oversight voids
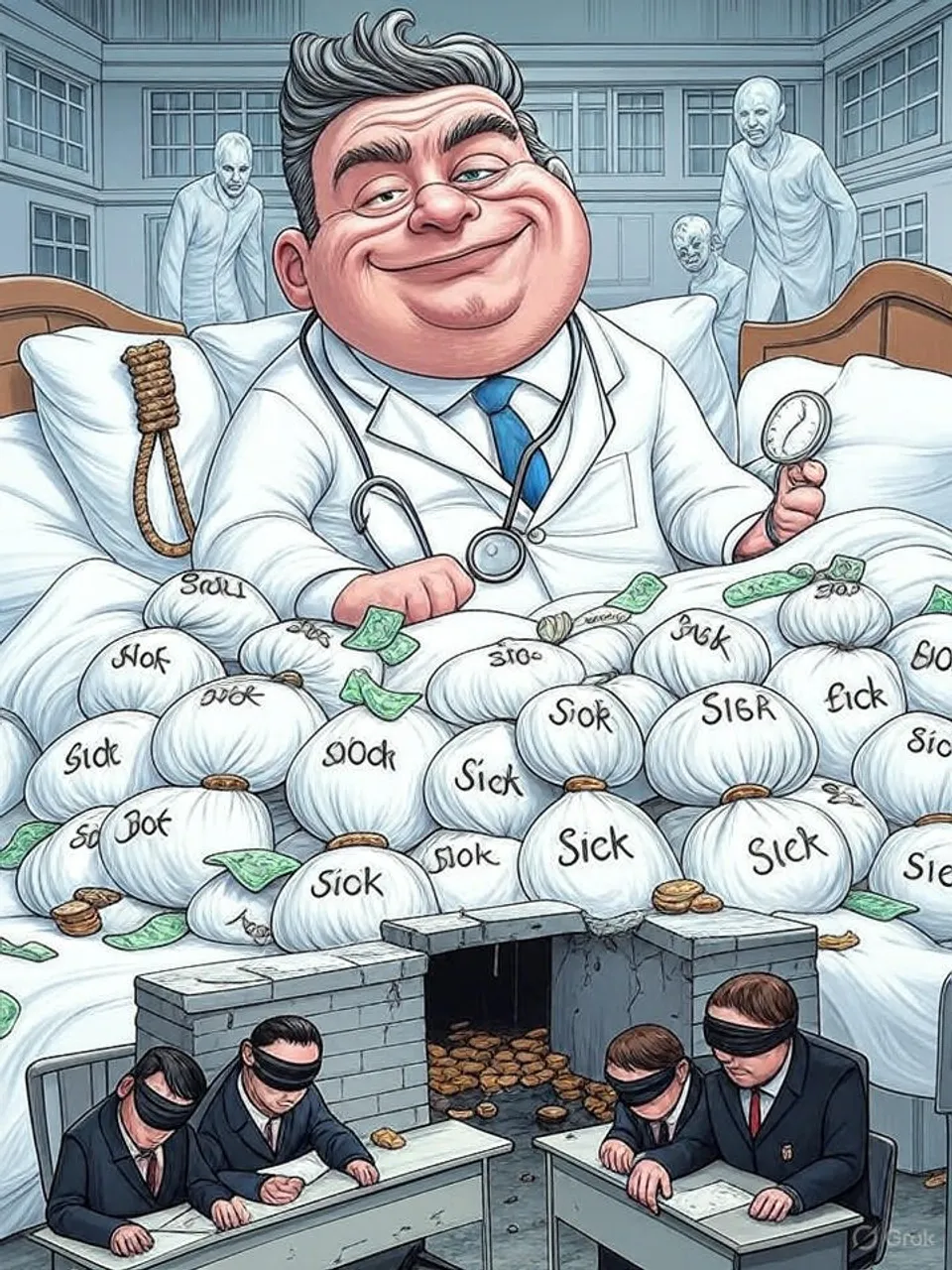
A doctor's three-year fraud of working extra shifts while claiming illness cost the NHS £268,000 in salaries and locums, exposing fragmented controls that enable abuse across trusts.
Commentary Based On
My London
Lying London doctor scammed £268K by working at other hospitals while claiming he was sick
A London obstetrician defrauded the NHS of £268,000 over three years by claiming sickness at one hospital while pulling night shifts at others. King’s College Hospitals NHS Foundation Trust paid his full salary and hired locums to cover his absences, under the assumption of his unfitness for work. This breach exposed a vulnerability in the system’s reliance on self-reported health without rigorous verification.
Richard Akinrolabu, 61, held a specialist registrar post at Princess Royal University Hospital in Orpington from October 2018 to December 2021. He informed occupational health of his inability to handle on-call or night duties, securing reduced hours or sick leave. Yet payroll records from Basildon Hospital, Princess Alexandra Hospital, East Kent Hospitals, and Mid-South Essex NHS Foundation Trust confirmed he logged dozens of such shifts there, netting extra income without permission.
Detection came late, in November 2021, via an anonymous tip about his Basildon work. The trust’s counter fraud team then cross-checked timesheets and witness statements, uncovering the full pattern. Akinrolabu offered no comment during his June 2022 interview, leading to charges of four counts of fraud by false representation; he pleaded guilty in September and received a three-year sentence at Woolwich Crown Court.
The financial toll extended beyond his salary. Locum doctors, often at premium rates, filled his gaps at King’s College, diverting funds meant for patient care. Judge David Miller noted the public’s expectation that doctors uphold truth, not exploit it—a standard this case shattered without immediate safeguards.
This incident fits a pattern of NHS fraud losses totaling £1.25 billion annually, per the NHS Counter Fraud Authority’s estimates. Akinrolabu’s scheme thrived on fragmented oversight across trusts, where secondary employment requires approval but lacks centralized monitoring. No single body tracks doctor workloads in real time, allowing such dual roles to persist undetected.
Historical comparisons underline the decay. In the 1990s, NHS staffing operated under tighter regional controls, with manual checks limiting such abuses. Today, post-2012 fragmentation into foundation trusts has multiplied administrative silos, weakening accountability even as workloads ballooned during the pandemic.
Patients bear the indirect cost. Resources squandered on locums—estimated at double a regular doctor’s pay—strain an already overstretched service facing 7.6 million waiting lists. Akinrolabu’s actions, while individual, exploit systemic gaps that governments of all stripes have failed to close, from Labour’s 2000s expansions to Conservative efficiency drives.
Enforcement remains reactive. The NHS Counter Fraud Authority pursues cases like this, but prevention relies on trust-grade doctors self-regulating amid burnout rates exceeding 50%. Without mandatory digital payroll integration or AI-flagged anomalies, similar frauds recur, eroding the service’s core compact with the public.
Cross-party neglect amplifies the issue. Labour’s 2024 pledges for NHS reform sidestep fraud controls, while prior Tory austerity cut investigative teams by 20%. Officials rotate roles without consequence, leaving root causes—understaffing and siloed data—unaddressed.
This fraud reveals the NHS as a sieve for public money, where professional oaths yield to personal gain under lax supervision. Britain’s healthcare system, once a global benchmark, now documents its own decline through such betrayals, diminishing care for millions while trust in institutions frays further.
Commentary based on Lying London doctor scammed £268K by working at other hospitals while claiming he was sick by Chris Ballinger on My London.