When Medical Evidence Takes a Back Seat to Cultural Politics
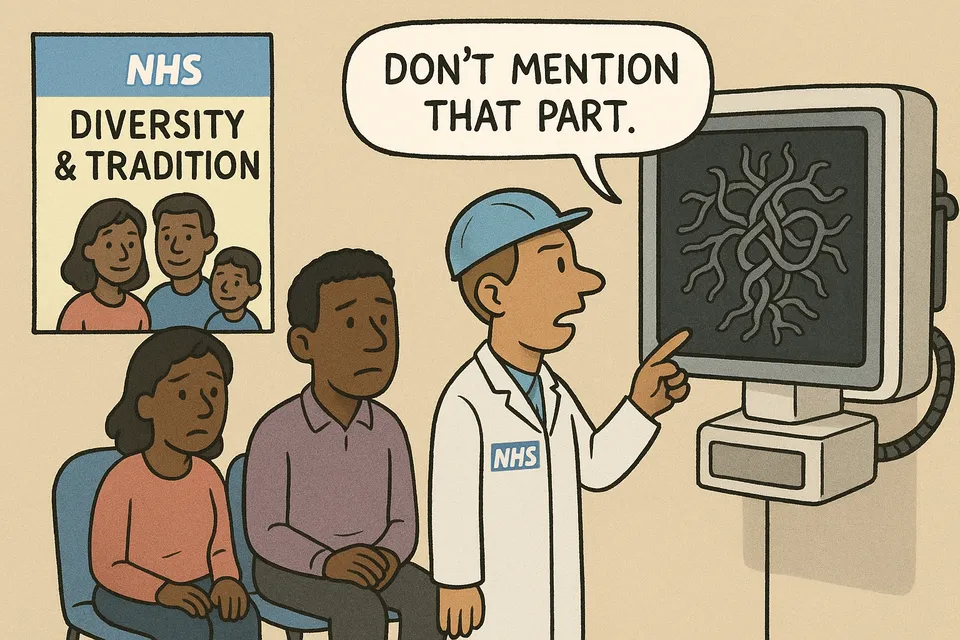
NHS guidance on cousin marriage prioritizes cultural sensitivity over genetic risk
Instead of providing clear medical advice, the NHS has issued guidance that downplays the genetic risks of first-cousin marriage by emphasizing its cultural and economic "benefits." This reflects a troubling trend where political correctness overrides scientific evidence in public health policy.
Commentary Based On
Telegraph
First-cousin marriages has ‘benefits’, says NHS guidance despite birth defect risk
The NHS has published guidance claiming first-cousin marriage offers “economic advantages” and “stronger family support systems” while acknowledging the practice increases genetic disorders in children. This isn’t medical guidance. It’s institutional surrender dressed up as cultural sensitivity.
The Facts That Matter
NHS England’s Genomics Education Programme published guidance last week that reads like a sociology paper rather than health advice. The document acknowledges that children of first-cousin marriages face increased risk of genetic conditions including sickle cell disease and cystic fibrosis. Then it pivots to discussing the practice’s “benefits” - stronger extended families and economic advantages.
When confronted, NHS England claimed the article was merely “a summary of existing scientific research” and not “expressing an NHS view.” Yet it appears on an official NHS education platform, funded by taxpayers who presumably expect medical guidance from their health service, not cultural apologetics.
The guidance even attempts historical justification, noting the practice has been legal since Henry VIII needed a loophole to marry his ex-wife’s cousin. As if a Tudor monarch’s marital arrangements constitute sound basis for modern public health policy.
The Pattern of Institutional Paralysis
This episode exemplifies a broader institutional decay: UK public bodies increasingly unable to state uncomfortable medical facts without immediately cushioning them with cultural relativism. The NHS guidance performs linguistic gymnastics to avoid stating the obvious - that a practice which increases genetic disorders in children is, from a public health perspective, harmful.
Consider what the NHS doesn’t equivocate about: smoking causes cancer, excessive drinking damages your liver, obesity increases heart disease risk. These statements appear without lengthy disclaimers about the cultural significance of pub culture or the economic benefits of the tobacco industry. Yet when genetic evidence collides with cultural sensitivities, suddenly the health service discovers nuance.
The guidance notes that alcohol, smoking, and parental age also increase health risks “none of which are banned in the UK” - as if the question was about legality rather than medical advisability. The NHS runs extensive campaigns against smoking and excessive drinking. It doesn’t publish documents exploring their “benefits.”
Why Medical Institutions Can’t Do Medicine Anymore
Dr Patrick Nash of the Pharos Foundation called the guidance “deeply misleading” and demanded retraction with apology. He won’t get one. UK institutions have developed a reliable pattern: publish something controversial, claim it’s been misunderstood when challenged, refuse to retract, wait for the news cycle to move on.
The real revelation isn’t that first-cousin marriage carries genetic risks - medical science established that decades ago. It’s that Britain’s premier health institution felt compelled to balance those risks against “economic advantages” and “family support systems.” Since when did the NHS become an arbiter of family economics rather than public health?
This represents institutional capture of a particularly British variety. Not by money or political parties, but by a paralysing fear of offending anyone, anywhere, about anything. The result: institutions that can no longer perform their basic functions without endless caveats, contextualizations, and contradictions.
The Costs of Comfortable Lies
The genetic risks are measurable. Studies consistently show children of first-cousin marriages face doubled risk of congenital abnormalities - from roughly 3% in the general population to 6%. In communities where the practice is common across generations, these risks compound. Bradford’s Born in Bradford study found that Pakistani-origin babies, where first-cousin marriage rates approach 60%, account for 30% of children with genetic disorders despite being 20% of births.
These aren’t cultural judgments. They’re mathematical realities that don’t change regardless of how many “benefits” the NHS lists. Every child born with preventable genetic conditions represents a failure of public health messaging prioritizing cultural comfort over medical truth.
The NHS spends millions treating genetic conditions that increase with consanguineous marriage. The same institution publishing this guidance will treat the consequences - managing chronic conditions, providing special education support, funding lifelong care. Taxpayers fund both the misleading guidance and its medical consequences.
When Everything Becomes Politics
Richard Holden MP linked the issue to immigration policy, demanding Labour “ban a practice the overwhelming majority, from every community in Britain, want to see ended.” This partisan framing obscures the deeper institutional failure. The problem isn’t which party controls government - it’s that medical institutions no longer feel capable of stating medical facts without political mediation.
The NHS guidance warns against “stigmatising certain communities and cultural traditions.” But what about stigmatizing medical professionals who want to give clear health advice? What about the children born with preventable conditions because their parents received mixed messages from health authorities more concerned with cultural sensitivity than genetic reality?
The Bigger Decline
This NHS guidance represents British institutional decline in microcosm: the inability to state simple truths, the elevation of political considerations over professional expertise, the institutional doublespeak that claims documents published on official platforms don’t represent official views.
Britain once pioneered public health campaigns that changed global behavior around smoking, workplace safety, and disease prevention. The same country that invented the randomized controlled trial now publishes health guidance that reads like a cultural studies essay, complete with genuflections to “cultural traditions” that increase childhood genetic disorders.
The decline isn’t that first-cousin marriage exists - it’s that the institution charged with protecting public health can’t bring itself to say clearly that the practice harms children. Instead, it publishes documents exploring “benefits” while hoping no one notices the contradiction between medical evidence and political messaging.
When health services can’t provide health advice without cultural caveats, when medical facts require political balance, when genetic counseling includes economic analysis - that’s not cultural sensitivity. It’s institutional cowardice. And the price is paid by children born with preventable conditions while adults argue about whether it’s culturally appropriate to prevent them.
The NHS guidance will remain online, neither endorsed nor retracted, existing in that peculiarly British institutional space where nothing is quite what it claims to be and nobody is quite responsible for anything. Another small surrender in the long retreat from institutional competence, documented with all the “benefits” carefully listed and the costs quietly ignored.
Commentary based on First-cousin marriages has ‘benefits’, says NHS guidance despite birth defect risk by Joe Pinkstone on Telegraph.