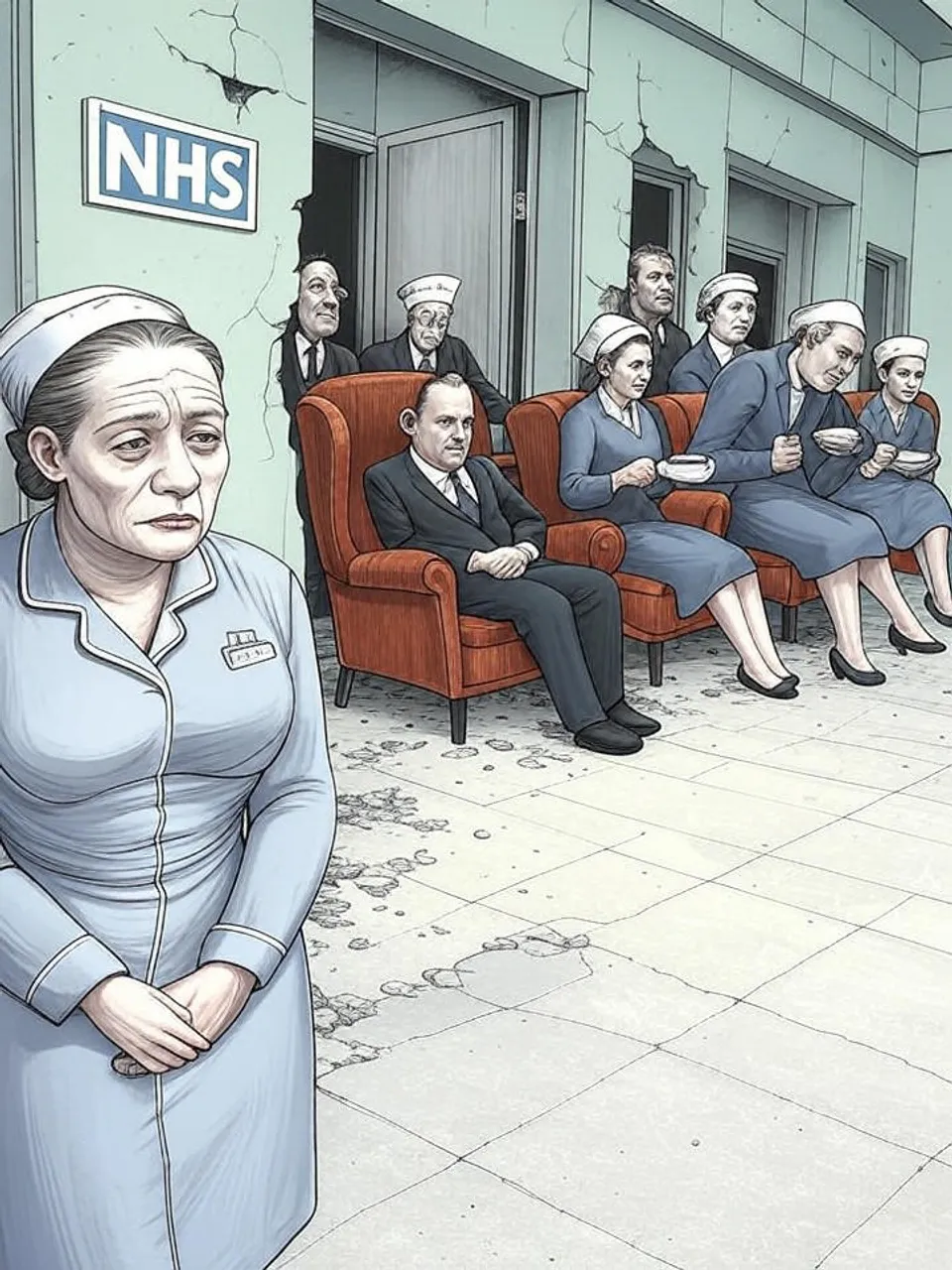
Nurses Clock In Despite Collapse
66 Percent Work Through Illness Amid 25,000 Vacancies
A surge in nurses working unwell exposes NHS understaffing's toll, with stress up 15 points since 2017. Cross-party failures lock in a broken system, eroding care and workforce resilience.
A Royal College of Nursing survey reveals that 66 percent of UK nurses have worked while unfit for duty, a sharp rise from 49 percent in 2017. This figure underscores a health service where staff prioritize patient loads over personal recovery, driven by chronic understaffing. Official narratives of workforce support clash with evidence of deepening exhaustion.
The survey polled over 20,000 nursing staff. Respondents reported 65 percent attributing illness primarily to stress, up from 50 percent eight years prior. Seven in ten nurses exceed contracted hours weekly, with half of those instances unpaid.
These patterns trace to persistent vacancies. England alone faces over 25,000 unfilled nursing posts. Under-resourced wards force individuals to cover for absent colleagues, turning routine shifts into endurance tests.
Staff accounts expose the human toll. One nurse developed a chronic stress-related illness but stayed on duty to avoid burdening an overwhelmed department. Another in a care home dreaded short-staffed days, knowing overtime would stretch unpaid into nights.
The Royal College of Nursing fields six daily calls from members on staffing crises, projecting 2,175 by year-end—up from 1,837 in 2023. Burnout manifests in panic attacks and nightmares. This volume signals not isolated incidents but systemic overload.
NHS leaders acknowledge the strain. They highlight nurse advocates and a graduate guarantee placing thousands of new staff. Yet vacancies persist, and the survey shows no relief in frontline pressures.
Government Promises Versus Ward Realities
The Department of Health and Social Care points to a 10-year plan for better conditions. It inherited an overworked force, officials claim, and now eases access to new roles. Implementation lags, however, as stress metrics climb unabated.
This disconnect repeats across administrations. Labour’s 1997 pledges boosted NHS funding initially, but by 2010, vacancies hovered at 10,000. Conservative austerity from 2010 widened gaps to 40,000 by 2019; the pandemic accelerated the exodus.
No party has reversed the trend. Post-2017 data shows acceleration under both Tory and Labour governments. The result: a workforce shrinking against rising demand from an aging population.
Patient care suffers in silence. Overloaded nurses manage dozens, sometimes over a hundred patients per shift. Errors rise, outcomes worsen, yet official reports emphasize recruitment wins over retention failures.
Economic costs compound the crisis. Unpaid overtime drains personal finances while inflating NHS budgets indirectly. Lost productivity from illness feeds into broader labor shortages, with nursing mirroring declines in teaching and policing.
Institutional Inertia at Work
Accountability evades capture. Chief executives rotate amid scandals, but frontline fixes stall. Unions demand investment, yet budgets prioritize administration over beds.
Historical benchmarks highlight the slide. In 2000, nurse-to-patient ratios allowed breathing room; today, they strain under 1:8 in acute settings. This erosion reflects policy choices favoring tax cuts or bailouts over core services.
Citizens bear the fallout. Wait times lengthen, with 7.6 million on elective lists as of mid-2024. Ordinary families face delayed treatments, while staff sacrifice health for the system.
The nursing survey lays bare a health service in freefall. Decades of cross-party neglect have forged an NHS where workers break before institutions bend. Britain’s decline manifests here: public assets hollowed out, leaving citizens exposed to unmanaged decay.
Commentary based on Two-thirds of nurses in UK work while unwell, says union by Tobi Thomas on The Guardian.